

NURSE ENTREPRENEUR
Nurse Influencer: Dementia & Mental Health
Rekha Boodoo-Lumbus brings over 25 years of cross-sector experience to her role as an Independent Nurse Specialist, with a dedicated focus on mental health and dementia. As founder of Rakhee LB Limited, she provides compassionate, tailored support to families, carers, and professionals, bridging clinical expertise with humanitarian purpose and relational clarity.
Her work is rooted in behavioural science, drawing from anthropology, psychology, psychiatry, and neuroscience to address the complex realities of dementia care. Rekha’s initiatives include the creation of Dementia Mauritius, a Nurse-led Holistic Dementia Clinic, and multiple peer-led support groups, all designed to promote dignity, wellbeing, and community empowerment. She also brings a strong foundation in research and data analysis, using visualisation and behavioural insight to inform care pathways and strategic decision-making.
Beyond clinical care, Rekha is known for her consultancy work, civic advocacy, and leadership rooted in compassion and strategic clarity. She engineers clarity across digital and physical spaces, offering strategic guidance to organisations, stakeholders, and families navigating care systems. Her practice is grounded in trust, transparency, and a deep respect for lived experience and human dignity.

OUR SERVICES
Values and Ethical based Leadership

Advocacy
Our goal is to empower you to take control of your wellbeing. We do this by protecting your rights and ensuring you access the right services, so you can make confident, informed choices that support your health and happiness.
Our Philosophy on Compassionate Leadership
We believe that true leadership in healthcare is compassionate and inclusive. Our work is driven by a shared vision to improve wellbeing for both people and communities. We actively reduce barriers and health disparities by valuing difference and committing to equity, diversity, and inclusion in everything we do


From Influencer to Empowerment
We believe that true influence comes from a dedication to learning, integrity, and excellent communication. By combining these insights with a clear vision, we can create meaningful change and empower others. We spread knowledge and generate empowerment through:
Clinical supervision
Peer supervision
Peer support groups
Values Driven Partnerships
Our partnerships are built on a foundation of integrity, respect, and trust. We believe these values are essential for creating meaningful change.
We form strategic collaborations to solve complex problems in community health and care. Our goal is to work with stakeholders across all sectors, from health and social care to community groups, to improve access to services for vulnerable populations dealing with dementia and mental health issues. We empower and coach our partners to ensure long-term success


Services
We offer specialised services for mental health and dementia, focusing on providing comprehensive and compassionate care for individuals and their families. We work together to create personalised treatment plans that address the unique needs of each person affected by dementia and/or mental health.
Comprehensive Assessments
We conduct thorough evaluations to identify the specific needs and challenges faced by individuals with mental health and dementia-related concerns.
Individualised Treatment Plans
Based on the assessment, we develop a tailored treatment plan that incorporate a holistic approach, e.g. medication advice, cognitive behavioural approach, and other supportive interventions.
Family Support and Education
We provide support and guidance to families and carers, helping them understand the condition and learn effective strategies for managing symptoms and promoting overall well-being.

Community Resources
We connect individuals and families with local resources, support groups, and community programs that can further enhance their quality of life.
Ongoing Monitoring and
Follow-Up
We regularly monitor the progress of each individual and adjust their treatment plan as needed to ensure the best possible outcomes.
With the support of services already involved.
Telemedicine
Digital technologies to deliver services remotely. This can include virtual consultations, remote monitoring, and digital communication between patients, and their families to provide support and advice. It can be used to treat a wide range of conditions, including mental health issues such as depression, anxiety, and stress.



Dementia Mauritius
Building a Psychosocial Education Platform
Since 2020, our mission has been to provide unwavering support to individuals living with dementia, their families, and dedicated carers. Through advocacy, personalised advice, and compassionate care, we’ve fostered a community that champions dignity, safety, and holistic wellbeing. Into the heart of our journey: Our focus is to create a psychosocial education platform that helps people understand Dementia and Alzheimer’s disease. By raising awareness, providing support, and engaging families, we can navigate this challenging journey together.
Compassion and knowledge are our allies in the fight against dementia.
01
Advocacy: Amplifying Voices
Advocacy lies at the core of our work. We have tirelessly raised awareness about dementia, dispelling myths and misconceptions. Our campaigns have reached some schools, workplaces, community centres, and charities emphasising early detection and reducing stigma. By amplifying the voices of those affected, we have sparked conversations that matter.
03
Dignity: Honoring Personhood
Dementia does not erase identity. We honour each person’s unique history, preferences, and passions. Our “Individualised Life Story” sessions celebrate life milestones, creating connections beyond memory loss. Dignity lies in acknowledging the person behind the diagnosis.
05
02
Empowerment: Nurturing Independence
Dementia need not diminish one’s autonomy. We empower individuals by fostering self-reliance. Our workshops focus on memory-enhancing techniques, adaptive strategies, and maintaining cognitive function. We celebrate small victories - a cherished memory recalled, a familiar face recognised - as steps toward empowerment.
04
Palliative Care and End of Life Support
In the twilight hours, we stand by families. Palliative care is not just about symptom management; it is about emotional solace. We facilitate open conversations, respecting individual wishes. Our bereavement support extends beyond loss, celebrating lives well-lived.
Frailty: Navigating Complex Needs
As dementia progresses, frailty becomes a concern. We address nutritional needs, physical activity, and emotional well-being. Additionally, we work alongside palliative care specialists and/or pain clinic to enhance comfort and maintain a high quality of life.

Mrs. X, an 81-year-old living with Alzheimer's and worsening mental health, faced significant challenges with daily tasks and social isolation. To support her and her family, we implemented a comprehensive, multidisciplinary approach.
This collaborative plan included:
-
Multidisciplinary Team: Coordinated care from physicians, nurses, and social workers.
-
Targeted Support: Effective medication management, social activities, and home safety adaptations.
-
Carer Assistance: Resources and guidance to alleviate family stress.
By addressing all aspects of her care, we improved her well-being, respected her wishes through advance care planning, and empowered her family to provide better support.
Mental Health and Cancer: Improving Care and Support
Ms. Smith, 56, was facing a dual battle with breast cancer and worsening depression. The challenges of treatment, coupled with increasing social isolation, led to significant stress and burnout for her and her family carers.
Our Holistic Approach: A collaborative, multidisciplinary care plan was implemented to provide comprehensive support. This included:
-
Integrated Care: Bringing together medical and mental health experts.
-
Targeted Support: Effective medication management, social engagement, and home safety guidance.
-
Caregiver Resources: Providing essential support to reduce family stress.
This approach successfully improved Ms. Smith's well-being and empowered her family to provide the best possible care.
Dementia and Mental Health: Improving Care and Support
Case Study
Lewy Body Dementia and Cancer: Improving Care and Support
Mr. Smith, 72, was facing a dual battle with lung cancer and worsening Lewy body dementia. The challenges of treatment, coupled with increasing social isolation, led to significant stress and burnout for him and his family caregivers.
Our Holistic Approach: A collaborative, multidisciplinary care plan was implemented to provide comprehensive support. This included:
-
Integrated Care: Bringing together medical and mental health experts.
-
Targeted Support: Effective medication management, social engagement, and home safety guidance.
-
Caregiver Resources: Providing essential support to reduce family stress.
This approach successfully improved Mr. Smith's wellbeing and empowered his family to provide the best possible care.

Our personalised treatment plans are designed to meet the unique needs of each person. Below is an overview of the services we offer, including our new Sitting and Befriending Service, available exclusively in the Bristol area. Pricing is provided upon enquiry. All fees are tailored to individual needs and circumstances.
Consultations & Interventions
We offer a range of support tailored to your needs, from initial conversations to in-depth sessions.
o. Free Initial Consultation: 30-45 minutes, a chance for us to understand your needs.
o. Follow-up Consultation: 30 minutes
o. Extended Consultation: 60 minutes
Talk-Based Session:
o. Standard Letter
o. Detailed Report
o. Comprehensive Assessment Report
Letters & Documentation
Professional written support to assist your care journey.
o. Standard Letter
o. Detailed Report
o. Comprehensive Assessment Report
Sitting & Befriending Service
(Bristol Area Only)
Compassionate companionship and practical support for individuals who may benefit from a reassuring presence.
o. Hourly Rate
o. Half-Day Service
o. Full-Day Service
Financial Considerations
We believe that everyone deserves quality care. If you need support. Please contact us to discuss your specific needs in a confidential conversation.
MEDIA CENTRE
Here’s What’s Happening
NATIONAL CONTEXT
In the UK, the number of people living with dementia is estimated to be over 982,000, with that figure projected to surpass one million by 2030. An estimated 540,000 carers in England alone support individuals with dementia. A recent report by the Alzheimer's Society highlights that many people affected by dementia receive no health, social, or financial support, and fewer than half are satisfied with the support they do receive.
Regarding mental health, approximately 2.8 million people were in contact with NHS-funded services in 2024/25. This includes specific services for children and young people, with 829,308 under-18s receiving care in that period. There has also been a significant increase in the number of women accessing specialist perinatal mental health services, rising to 63,784 in 2024/25.
Areas of Expertise & Professional Focus
My work is driven by a passion for holistic, person-centred care and a commitment to global health. I lead and contribute to initiatives that bridge clinical practice with innovative community solutions.
Research & Clinical Initiatives
These projects focus on improving care through a blend of research, quality improvement, and innovation, addressing unique and often overlooked challenges.
-
Holistic Care Models: Developing interdisciplinary and transdisciplinary approaches to person-centred care.
-
Post-Diagnostic Support: Exploring post-diagnostic support for mental health and dementia in overseas countries, identifying key barriers and opportunities.
-
Complex Health Needs: Investigating the link between visual impairments and mental health problems in older adults, and addressing the specific challenges of Posterior Cortical Atrophy (PCA) and access to psychological support.
-
Wound Management: Researching the usability characteristics required for effective wound management and tissue viability.
Global & Community Strategy
This work extends beyond traditional clinical settings to reduce health disparities and improve care for entire communities.
-
Global Impact: Exploring the worldwide impact of dementia and mental health, with a focus on creating community initiatives and policies to reduce the global burden of these disorders.
-
Community-Based Strategy: Developing a comprehensive community-based dementia strategy, from pre-diagnosis and palliative care through to end-of-life support.
-
Nurse-Led Clinics: Shaping the future of care by embracing a holistic and strategic approach through nurse-led clinics.
Professional Development & Mentoring
A core part of my mission is to advocate for a culture of continuous learning and growth within the healthcare profession.
-
Fostering Innovation: Leading initiatives to foster a culture of research, quality improvement, and innovation among peers.
-
Professional Networking: Actively networking with nurses and other healthcare professionals globally to share knowledge and build collaborative relationships.
-
Reverse Mentoring: Promoting personal and professional development through advocacy and reverse mentoring.


Helpful Resources & Interesting Findings

We believe that knowledge empowers. That’s why we have curated a selection of key studies, guides, and resources to help you stay informed on the latest developments in mental health and dementia care.
Key Findings
-
Mental Health and Dementia: Research shows a strong association between mental health conditions and the later development of dementia, suggesting that addressing mental health issues can play a role in prevention.
-
Mind-Body Connection: Explore how mindfulness-based practices and other mind-body approaches can help improve both mental and physical well-being.
-
Delirium in ICU Patients: A new study highlights the link between a patient’s mental health-related quality of life and the likelihood of experiencing delirium in intensive care.
Guides for Carers
-
Eating and Drinking Well with Dementia: A guide for caregivers on managing nutritional needs.
-
Arts & Dementia: A pocket guide on using art to improve the quality of life for individuals with dementia.
-
Pet Therapy: Learn about the benefits of companionship and pet therapy for the elderly.

Our Foundational Values
At Rakhee LB, our work is more than a service, it is a commitment to a set of core values. We believe that health is true wealth and that everyone matters. Our work is guided by these principles, which enable us to promote long-term relationships built on trust and respect. We embody a spirit of initiative, continuously innovating to improve care. Our profound sense of service ensures every action is tailored to the individual. Above all, we stand by our commitment to support social and societal changes that benefit our communities.
Our Core Values:
-
Respect: We value your unique story and recognise the dignity of every person.
-
Trust: We earn your confidence and build long-term relationships through transparency and honesty.
-
Service: We personalize our care to guarantee the quality and relevance of our actions.
-
Initiative: We innovate for your future, always anticipating how to improve care.
-
Commitment: We are here for you and our community, dedicated to driving positive social change.

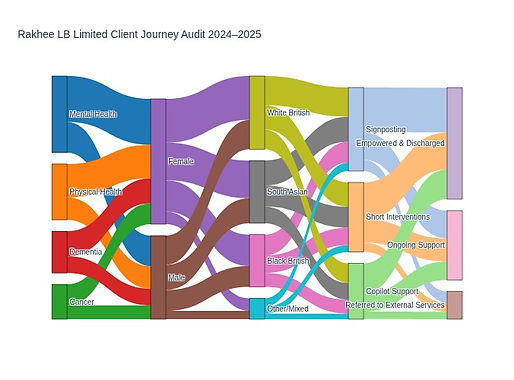
Client Engagement Overview: Dual Sankey Diagrams
(Oct 2024–Sept 2025)
.jpeg)
🧭Framing Statement for Dual Sankey Diagrams
To reflect the evolving nature of client engagement at Rakhee LB Limited, two Sankey diagrams have been developed. One focuses on clients who received Copilot support, showcasing the role of digital assistance in service navigation and emotional wellbeing. The other highlights those who accessed traditional or community-based support, offering insight into more conventional care pathways. Together, these visuals present a complete picture of how individuals engage with services, digitally and face-to-face, without overlapping content or duplicating narrative.
🔗 Sankey Diagram 1: Copilot-Supported Engagement
This diagram illustrates how clients interact with Copilot as part of their care journey. It begins with their initial health concern, such as mental health, physical conditions, cancer, or dementia and branches into demographic details like sex and ethnicity.
From there, it shows how clients use Copilot for:
-
Navigating available services
-
Receiving emotional and cognitive support
-
Accessing clear, jargon-free information
-
Engaging in digital routines and reminders
The final branches reflect outcomes such as:
-
Greater confidence in self-navigation
-
Reduced emotional distress
-
Improved service uptake
-
Referral to human-led support when needed
Visual elements include:
-
Colour-coded diagnosis streams
-
Shaded overlays for sex
-
Patterned segments for ethnicity
-
Quotes and vignettes to humanise the data
✅ Sankey Diagram 2: Traditional & Community-Based Support
This second diagram follows clients who engaged with non-digital services. It mirrors the same diagnostic and demographic entry points but focuses on pathways like:
-
Signposting to relevant services
-
Short-term interventions
-
Support from staff, carers, or community partners
Outcomes include:
-
Empowerment and discharge
-
Continued support
-
External referrals
Design features remain consistent for clarity, with distinct annotations that highlight individual stories and feedback. These include:
“I didn’t know where to start, but the team helped me understand my options.”
“The dementia support helped my mum and helped me feel less alone.”
“After the short sessions, I felt more in control of my anxiety.”
“They explained everything clearly and helped me get the right benefits.”
“I was signposted to housing support and things finally started to move forward.”


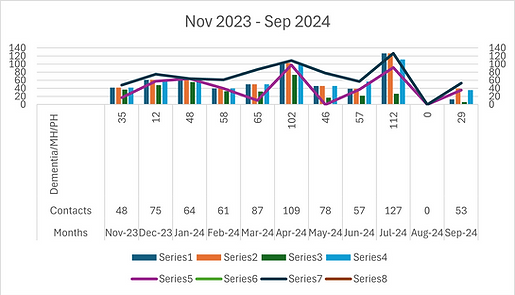


Report on Data Analysis and Visualisation - Complex Cases
November 2023 - September 2024
Introduction
This report provides an analysis of the data represented in three graphs covering the period from November 2023 to September 2024. The graphs illustrate various categories and series, highlighting trends and patterns over time. The effort involved in capturing and visualising this data is also discussed.
Graph 1: 3D Clustered Bar Chart
Description
The first graph is a 3D clustered bar chart displaying data for several categories: Contacts, *Dementia/Mental Health/Physical Health, Support, Signposting, Interventions, Discharge Follow-up, Feedback, and Total. The vertical axis represents quantity, ranging from 0 to 140, while the horizontal axis covers the months from November 2023 to September 2024.
Findings
Contacts and Total: These categories consistently show higher values compared to others, indicating a significant volume of interactions and overall activity.
*Dementia/MH/PH Support: This category shows a steady trend, reflecting ongoing support needs.
Interventions and Feedback: These categories have moderate values, suggesting regular but less frequent activities compared to Contacts, mainly due to less complex cases.
Signposting and Discharge Follow-up: These categories have values, indicating that service users needed different services or interventions, and it was essential that they were directed to relevant services.
Graph 2: Bar and Line Graph
Description
The second graph is a combination of bar and line charts, titled “Nov 2023 - Sep 2024.” It includes eight series, each represented by different coloured bars and lines. The vertical axis is labelled “Demand in MH/PH,” with values ranging from 0 to 160.
Findings
Series Trends: Each series shows varying demand over the months, with some series peaking at different times. The lines connecting data points help visualise these trends clearly.
Demand Peaks: Certain months show higher demand for specific series, indicating periods of increased activity or need.
Graph 3: Bar and Categorised
Description
Categories: It includes three categories: Increase, Decrease, and Total. The Increase category is represented in light blue, Decrease in orange, and Total in dark blue.
Vertical Axis: The vertical axis represents quantity, ranging from 0 to 800.
Findings:
Increase and Total: Both categories show consistent growth over time, with the Total category reaching slightly above 700 at point 11.
Decrease: There are no bars for the Decrease category, indicating no recorded decreases during this period.
Data Collection and Visualisation Effort
Data Collection
Sources: Data was collected from various sources, including internal records, surveys, and external databases.
Validation: Ensuring data accuracy involved cross-referencing multiple sources and validating entries.
Frequency: Data was collected monthly to capture trends and changes over time.
Visualisation
Tools Used: Advanced data visualisation tools were employed to create the graphs, ensuring clarity and accuracy.
Design: The design process involved selecting appropriate chart types, colours, and layouts to effectively communicate the data.
Review: Multiple iterations and reviews were conducted to refine the visualisations and ensure they accurately represented the data.
Interventions
The data also reflects a combination of interventions, including:
Active Listening: Engaging with individuals to understand their concerns and needs.
Positive Reinforcement: Encouraging positive behaviour and progress.
Brief Cognitive Behavioural Therapy (CBT): Addressing specific issues through short-term, goal-oriented therapy.
Anxiety Management: Techniques to help individuals manage and reduce anxiety.
Risk Management through Third-Party Interventions: Collaborating with external organisations to manage risks.
Evaluation of Diagnosis and Post-Diagnosis: Assessing and following up on diagnoses to ensure appropriate care.
Benefits and Medication: Providing information and support regarding benefits, CHC, and medication management.
Conclusion
The analysis of the graphs provides valuable insights into the trends and patterns over the period from November 2023 to September 2024. The effort involved in data collection and visualisation was substantial, ensuring the accuracy and clarity of the presented information. These visualizations, along with the detailed interventions, serve as powerful tools for understanding and decision-making.

Nurse-Led Holistic Dementia Care: A Case Study in Impact
October 2022 - October 2023
Our Nurse-Led Holistic Dementia program focuses on providing targeted support to individuals living with dementia and their carers. By adopting a compassionate and holistic approach, we addressed complex needs and delivered a comprehensive program through a consistent 15.5 hours per week of service.
The program's core goal was to address the diverse needs of both carers and individuals living with dementia, focusing on vital topics such as:
-
Cognitive impairment, anxiety, and depression
-
Culturally appropriate bereavement support
-
Employment, benefits, and inequality
-
Removing barriers and fostering open dialogue
Key Findings and Outcomes
The data from this period, as demonstrated in our graphs, shows that our evidence-based, multimodal, and multidimensional approach has been highly effective.
-
Improved Well-being: Our interventions have significantly improved outcomes for many service users, successfully addressing concerns and providing vital support.
-
Empowerment: Clients and their families gained a sense of acceptance and empowerment, successfully overcoming stigma and embracing a more positive outlook.
-
Positive Community Impact: By fostering empathy, respect, and dignity through education and compassionate care, we helped reduce existing prejudices in the community.
This case study demonstrates the power of a nurse-led approach to transform the health and happiness of people living with dementia and those who care for them.


OPENING HOURS
Informal Questions
Monday - Friday: Varies
Saturday: 8am - 8pm
Sundays & Bank Holidays: Closed

CONTACT US
Get in Touch
We are here to help when you need us. While we do not have fixed operating hours, you can reach out anytime and we will respond as soon as possible.
📧 Email: Send us an email with your inquiry.
📞 Phone: Call us to schedule an appointment.
🌐 Online: Fill out the contact form below.
+44 7464100959
